I’m a pensioner and can’t afford dentures: what help does Australia offer?
Outline of the article
– Why affordable dentures matter for pensioners, and the funding landscape across Australia
– Public pathways: eligibility, waiting lists, and how to make the system work for you
– Support for veterans and other priority groups, including rural and disability considerations
– Training pathways through universities, including pros, cons, and costs
– Charity and community options, plus a step-by-step application checklist and final guidance
Introduction
Dental comfort isn’t a luxury; it shapes how we eat, speak, and smile. For many pensioners, though, the price of dentures can feel like a locked gate. The good news is that there are several doors to knock on—some public, some educational, some charitable—and each can lower the cost in different ways. This article is a practical map: it compares pathways, explains who qualifies, and shows how to prepare documents so applications move faster. Along the way, you’ll find small tactics that save real dollars and time, without compromising dignity or care.
Making the public system work for you on a pension
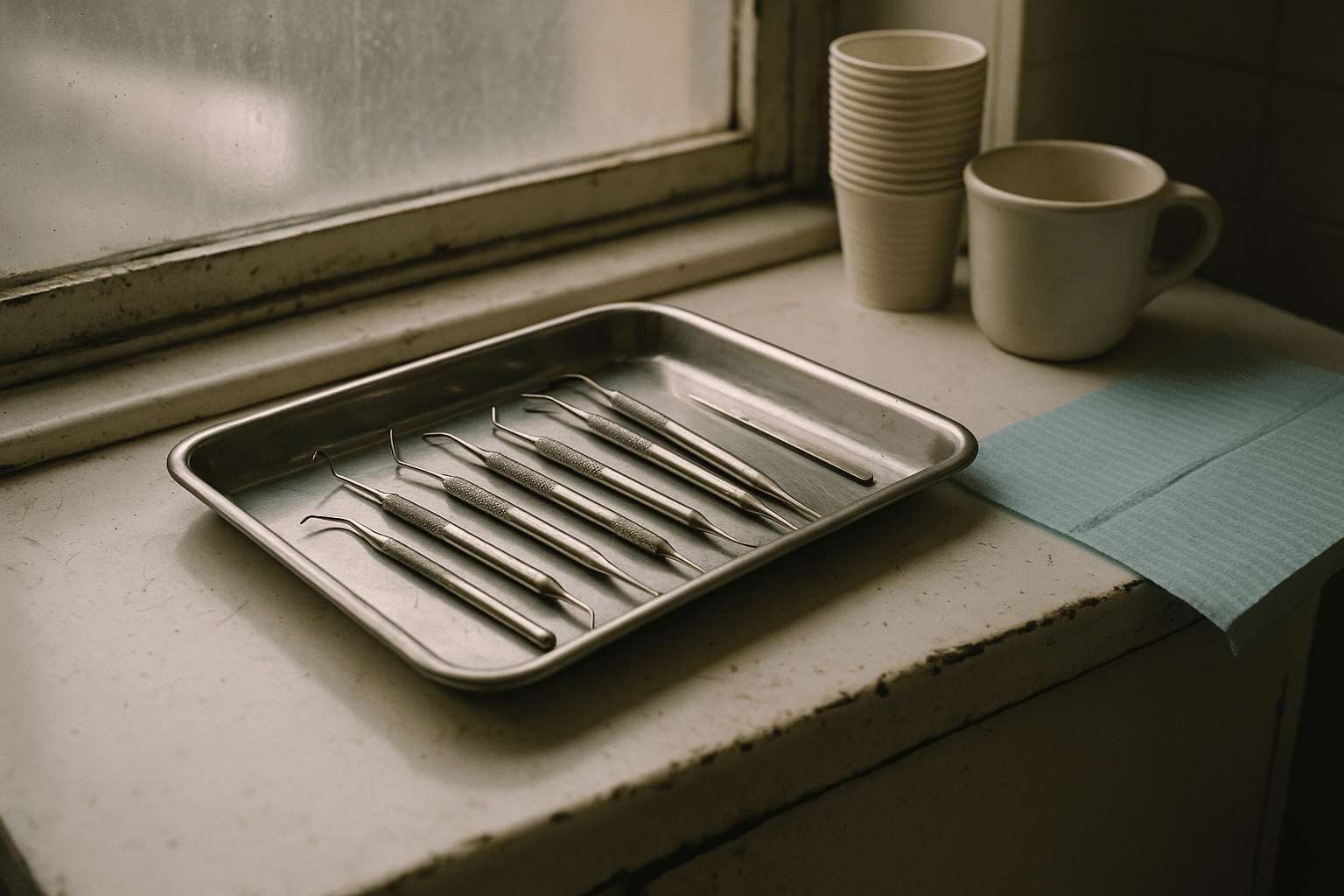
Across Australia, state and territory health systems offer clinics that can provide denture assessments, repairs, relines, and new appliances at subsidised rates. Eligibility commonly hinges on income, age, and residence, with priority often given to urgent needs—pain, infections, or significant functional issues. For many pensioners, this is the most direct route to care, but it can involve waitlists. Understanding how the system triages and what you can do to speed things up is essential. A key concept to ask about is Public dental services and concession-card support, because it is usually the gateway to fee reductions, vouchers, or priority access in certain circumstances.
What to expect typically varies by state or territory: some services run central booking lines; others rely on local clinics or community health centres. Co‑payments are often modest compared to private fees, but they may still apply. Emergency care can sometimes be accessed more quickly than routine denture work; however, if your dentures affect eating or social participation, you can explain the impacts to be assessed for priority.
When you call or attend an intake session, have a short script ready to explain your situation plainly. You might say you’re a pensioner, outline how the dentures affect your eating or speech, and mention any medical factors like dry mouth, diabetes, or medications that increase dental risk. A clear picture helps assessors place your case appropriately without overselling. Consider keeping notes of names, dates, and reference numbers, which makes follow‑ups smoother.
To maximise your chances of quick, affordable care, ask these questions upfront:
– Do I qualify under current concession rules and how do fees apply to me?
– Is there a waitlist, and what is the estimated time frame for denture services?
– Are there emergency or priority pathways if chewing or nutrition is affected?
– Can I be referred to a partner clinic if local capacity is limited?
– Is transport or travel assistance available for longer-distance appointments?
Finally, if you are placed on a waiting list, request written confirmation and ask how often the list is updated. Confirm whether periodic check‑ins help maintain your position, and whether you can accept short‑notice appointments. Many clinics welcome flexible patients who can attend quickly when cancellations appear, which can reduce waiting time without extra cost.
Support for veterans and people with additional needs
Beyond the general public pathway, there are targeted supports for those who served in the armed forces, as well as for people with disability, residents of aged‑care facilities, and those in remote or rural areas. The policy settings and paperwork differ, but the common thread is to demonstrate eligibility and clinical need in a clear, documented way. Understanding How veterans and special groups can access subsidised denture care can unlock entitlements that cover all or part of the treatment cost, sometimes including repairs, relines, and replacements after a reasonable interval.
Veterans may be eligible for fully or partially subsidised dentures through federally administered programs. Typically, you will need proof of veteran status and may require a referral from a recognised healthcare professional. If travelling is difficult, ask about telehealth triage or local providers approved to deliver care under veteran arrangements. Keep copies of prior dental records and any letters explaining why a new set or major repair is clinically indicated; clear documentation helps justify approvals.
For people with disability or complex health needs, public clinics often run dedicated sessions or have clinicians trained in special care dentistry. If you receive support through a care package or case management service, ask your coordinator whether funding can contribute to transport, accommodation for long trips, or additional appointment time. Residents of aged‑care facilities can sometimes access on‑site visits through outreach teams when transport is a barrier.
Aboriginal and Torres Strait Islander community health services may facilitate culturally safe pathways to denture care, navigating referrals and providing liaison support. In rural and remote regions, mobile teams and visiting practitioners can reduce long travel; if you are eligible, enquire about travel assistance schemes, which can offset costs like fuel or accommodation for the nearest clinic with denture capacity.
Key points to raise when you call:
– What documents prove my eligibility for veteran or special‑group support?
– Are there approved providers in my area and do I need a formal referral?
– What replacement intervals apply for lost or worn dentures?
– Is travel assistance or home‑visit care available where I live?
With the right referral pathway and paperwork, these targeted supports can shorten the journey from assessment to fitting, while keeping out‑of‑pocket costs manageable for those on fixed incomes.
Training clinics: how students and supervisors reduce costs
If you can be flexible with timing and appointment length, teaching facilities offer a strong value proposition. Supervised students gain experience, and patients benefit from reduced fees, detailed assessments, and careful step‑by‑step fabrication. Many pensioners find that University dental clinics as low-cost alternatives for denture treatment strike a practical balance: savings on fees in exchange for longer visits and a few more appointments than a private practice might require.
How it works: senior students or graduate trainees provide care under close supervision from qualified professionals. That means multiple checkpoints for fit, comfort, and bite. Appointments tend to be longer—plan for half‑day visits or multiple shorter sessions—so transport and energy levels should be considered when booking. The upside is a methodical process that often results in well‑fitting prostheses, with opportunities to ask questions at each stage.
Fee structures vary, but they usually reflect materials plus a reduced clinical charge. Some clinics also accept public referrals or vouchers that further lower costs. Waiting times can exist, especially at the start of academic terms, so it helps to register early and ask to be contacted if openings appear. If you currently wear dentures, bring them along; adjustments or relines might be viable interim steps while the new set is being planned.
Practical tips for teaching clinics:
– Ask how many appointments the process typically requires and the expected timeline.
– Confirm total costs, including any lab fees, and whether payment plans are offered.
– Enquire about priority criteria for patients with nutritional challenges or medical risks.
– Verify transport options, mobility access, and rest areas if lengthy visits are expected.
A candid trade‑off to consider: complex cases may be referred to specialized streams or senior cohorts, which can lengthen the timeline but may improve outcomes for challenging anatomy or long‑term bone changes. If you need a quicker fix, request a temporary reline or repair while the new dentures are made. This staged approach can keep you eating and speaking comfortably without straining your budget.
Charities, outreach, and community pathways
For some pensioners, the right door opens not at a large clinic, but at a pop‑up service in a community hall or a mobile van parked outside a library. These services aim to catch people who fall through the cracks—those who can’t travel easily, who face long waits, or who need a hand with forms and referrals. Charitable dental programs and community-based outreach options can include assessment days, repair clinics, voucher schemes, and partnerships with local health centres that refer patients to reduced‑fee denture providers.
While availability changes by region, the structure is similar: registered volunteers and qualified clinicians deliver focused services, often prioritising people experiencing homelessness, domestic upheaval, or sudden tooth loss affecting work or nutrition. Some programs emphasize repairs and relines because they stretch limited funds to help more people. Others run case‑by‑case grants to cover part of the cost of full or partial dentures when a public clinic wait is too long.
How to locate these services:
– Call your local council or community health centre and ask about dental outreach calendars.
– Check noticeboards at libraries, neighbourhood houses, and seniors’ hubs for upcoming clinics.
– Ask social workers, aged‑care coordinators, or multicultural support services about referral partners.
– Search for statewide helplines that maintain lists of low‑cost dental programs near you.
Reality check: capacity is finite, and appointments may fill quickly. Prepare for a first visit that focuses on assessment and eligibility rather than immediate treatment; this is not a brush‑off, but an efficient way to match limited resources to greatest need. If you’re flexible, leave your contact details for short‑notice openings. Also ask whether attending a public clinic intake first could strengthen your case for a support voucher—some programs coordinate closely, stretching funds further.
Even if a charity can’t fund a full set immediately, a reline or targeted repair can buy comfort and time while you progress through a public or training‑clinic pathway. Think of these services as stepping stones: small, timely interventions that keep you eating well and engaging socially as you work toward a lasting solution.
Your action plan: documents, applications, and a clear path forward
When money is tight, the straightest road is the one without surprises. That’s why it pays to gather the Practical steps and documents needed to apply for affordable dentures before you pick up the phone. Good paperwork reduces back‑and‑forth, speeds triage, and shows that you meet eligibility criteria. Here is a checklist you can tailor to your situation:
– Current concession card showing your name and expiry date
– Proof of address (recent utility bill or official letter)
– Proof of income or pension status (recent statement)
– List of medications and relevant medical conditions
– Any previous dental records, X‑rays, or denture details
– Referral letter, if required by a program you’re applying to
– Contact details for a support person who can assist with transport or communication
Step‑by‑step approach to lower costs and waiting time:
– Start with your state or territory public clinic intake line; ask about eligibility, co‑payments, and wait times.
– If dentures are impacting eating or speech, explain the specific effects and ask about priority assessment.
– Register with a nearby teaching clinic and request to be notified of cancellations.
– Contact a local community health centre or council to learn about upcoming outreach days and voucher programs.
– If you’re a veteran or belong to a priority group, call the relevant program line to confirm entitlements and referral requirements.
– Keep a simple folder—paper or digital—with all documents and notes from calls, including dates and names.
– Say yes to short‑notice appointments whenever possible to leapfrog delays.
Budgeting tips that help without strain:
– Set aside a small weekly amount toward lab fees so payments feel manageable.
– Ask about staged care: a reline now, a repair if needed, and a new set when a slot opens.
– Enquire whether travel assistance is available if the nearest clinic is far from home.
Conclusion for pensioners: You don’t need to tackle this alone, and you don’t have to choose only one path. Public clinics, veteran and priority programs, university training facilities, and community outreach can work together like pieces of a puzzle. With clear documents, a few well‑timed calls, and flexibility for short‑notice slots, you can move from uncertainty to a firm plan. Protect your nutrition, comfort, and confidence—the right support is closer than it seems, and every small step brings you nearer to a stable, affordable smile.